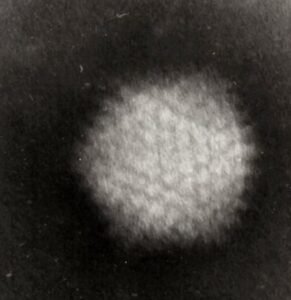
Aeromonas spp.
Aeromonas are Gram-negative bacilli, widely distributed in nature, especially aquatic environments – freshwater, brackish water, sewage system, hospital water system, and even drinking water. It can also be found in food and domestic or farm animals.
The Aeromonas genus consists of more than 30 species based on DNA-DNA hybridisation and 16S rDNA relatedness. Of these 30 species, 17 have been associated with human disease. However, only four species account for more than 95% of cases – Aeromonas caviae, Aeromonas dhakensis, Aeromonas veronii, and Aeromonas hydrophila,
Laboratory:
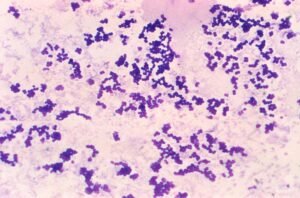
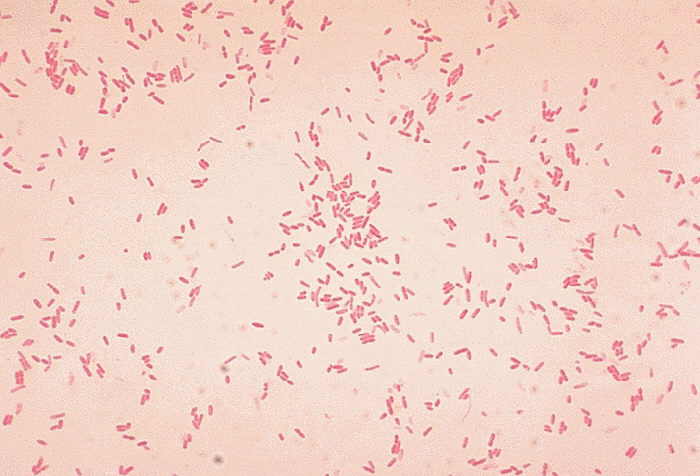
- Gram negative bacilli or coccobacilli.
- They are facultative anaerobe and easily grows on blood and Macconkey agar. They may or may not produce haemolysis on blood agar.
- Aeromonas are oxidase and catalase-positive, reduce nitrates to nitrites, and ferment glucose.
- It can be identified using API20E, MALDI-ToF and other commercial systems.
Differentiation from similar bacteria:
Plesiomonas and vibrio – Aeromonas are negative for ornithine decarboxylase hydrolysis (except for some A veronii).
Enterobacterales – Aeromonas are oxidase positive, enterobacterales are negative.
Sensitivity test
Intrinsic resistance:
Amoxicillin, ampicillin and ampicillin-sulbactam – intrinsically resistant.
Co-amoxiclav – EUCAST does not consider Aeromonas intrinsically resistant to co-amoxiclav. (Note – CLSI says Aeromonas is intrinsically resistant to co-amoxiclav)
Aeromonas dhakensis may have chromosomal ampC and resistance to cefoxitin.Some A caviae could be susceptible to ampicillin.
Aeromonas have multiple inducible chromosomal beta-lactamases and may develop resistance to cephalosporins on treatment. Some strains also have chromosomal carbapenemase production (A. jandaei, A. veronii biotype veronii and occasionally in A. hydrophila and A. dhakensis). *
EUCAST and CLSI have breakpoints for these antibiotics
| EUCAST | CLSI |
| Ceftazidime, cefepime, Aztreonam Ciprofloxacin, Levofloxacin Cotrimoxazole | Pip-tazobactam Cephems – cefepime, cefotaxime, cefoxitin, ceftazidime, ceftriaxone, cefuroxime (IV) Carbapenems – Doripenem, Ertapenem, Imipenem, Meropenem, Monobactam – Aztreonam Aminoglycoside – Amikacin, gentamicin Tetracycline Quinolone – Ciprofloxacin, levofloxacin Cotrimoxazole Chloramphenicol |
Aeromonas infection:
Aeromonas infection is often associated with the history of exposure to water (fresh, brackish, sewage, even treated water), leech therapy or consumption of raw or semi-cooked seafood. However, nosocomial infection associated with hospital water sources has been reported.Presenting features are skin and soft tissue infection, gastroenteritis, sepsis – usually in patients with immunocompromised state (malignancy, drugs), hepatobiliary disease, diabetes mellitus.
Common Aeromonas infections are bacteremia, hepatobiliary tract infections, and soft tissue infections.
| Bacteraemia | – Associated with underlying illnesses such as immunocompromised state (malignancy, immunosuppressive drugs, neutropenia), hepatobiliary disease and diabetes mellitus. – The most common portal of entry into the bloodstream is the gastrointestinal tract. – Case fatality could be 25-60%. |
| Biliary infection | – Associated with biliary obstruction due to stone or malignancy. – Spontaneous bacterial peritonitis with high mortality (50%) has also been reported. |
| Skin and soft tissue infection | – The role of Aeromonas in gastrointestinal illness is debatable. It has been isolated from patients with various types of diarrhoeal illness – acute watery diarrhoea, travellers diarrhoea, chronic diarrhoea, dysentery, but whether they are the pathogen has not been conclusively proven. – The disease is often self-limiting, but complications like haemolytic uraemic syndrome have been reported. |
| Gastrointestinal infection | – The role of Aeromonas in gastrointestinal illness is debatable. It has been isolated from patients with various types of diarrhoeal illness – acute watery diarrhoea, travellers diarrhoea, chronic diarrhoea, and dysentery, but whether they are the pathogen has not been conclusively proven. – The disease is often self-limiting, but complications like haemolytic uraemic syndrome have been reported. |
Other infections caused by Aeromonas are – pneumonia, especially associated with malignancy and drowning; eye infections like contact lens-associated keratitis; and genitourinary infection.
Virulence
Some Aeromonas are more virulent (A. dhakensis, A. hydrophila, or A. veronii) than others (A. caviae). Virulence factors are hemolysin, aerolysin, type III secretion system, siderophore, endotoxin, haemagglutinin etc.
Treatment
- Aeromonas is usually susceptible to 3rd or 4th generation cephalosporins, fluoroquinolone, cotrimoxazole, aminoglycosides, carbapenems, and chloramphenicol.
- Gastroenteritis is usually self-limiting.
- Cotrimoxazole or quinolones could be used for treatment. 3rd/4th gen cephalosporins are also used.
- Severe infections like necrotising fasciitis may need combination treatment.
Beta-lactamase produced by aeromonas
Aeromonas produces both chromosomal and plasmid or integron-mediated beta-lactamases.
Three chromosomally encoded beta-lactamases have been described –
| Ambler class | Enzyme | Where found | Note | |
| Ambler molecular class B (metallo-beta-lactamases, MBLs) | cphA | A. hydrophila, A. veronii, A. jandaei, A. dhakensis | Active against penems and carbapenems, but not against penicillins or cephalosporins. | |
| Ambler molecular class C (AmpC cephalosporins) | AsbA1, cepH, cepS, CAV1, TRU1, ACU1 | A. jandaei, A. hydrophila, A. caviae, A. enteropelogenes, A. dhakensis | It may not be expressed, and the organism may appear susceptible to 3rd gen cephalosporin. Beta-lactamase can induce production. The use of 3rd generation cephalosporin should be monitored carefully in cases where bacterial load is high. Mutation can derepress beta-lactamase production. | |
| Ambler molecular class D (penicillinases) | AmpH, AmpS | A. jandaei, A. hydrophila, |
Plasmid/ integron beta-lactamases
| Ambler Class | Example | Species | Note |
| Ambler class A | TEM-24, CTX-M-3, CTX-15, PER-1, PER-3, PER-6, SHV-12, VEB-1a, TLA-2, and GES-7 | Extended Spectrum beta-lactamases (ESBL). Rare | |
| Ambler Class B | IMP, VIM | A hydrophila A caviae | |
| Ambler Class C | CMY-1/MOX-family, FOX etc | Hydrolyse extended-spectrum cephalosporins and cephamycins, and moxalactam (MOX family) |