Plesiomonas shigelloides
Plesiomonas shigelloides characteristics
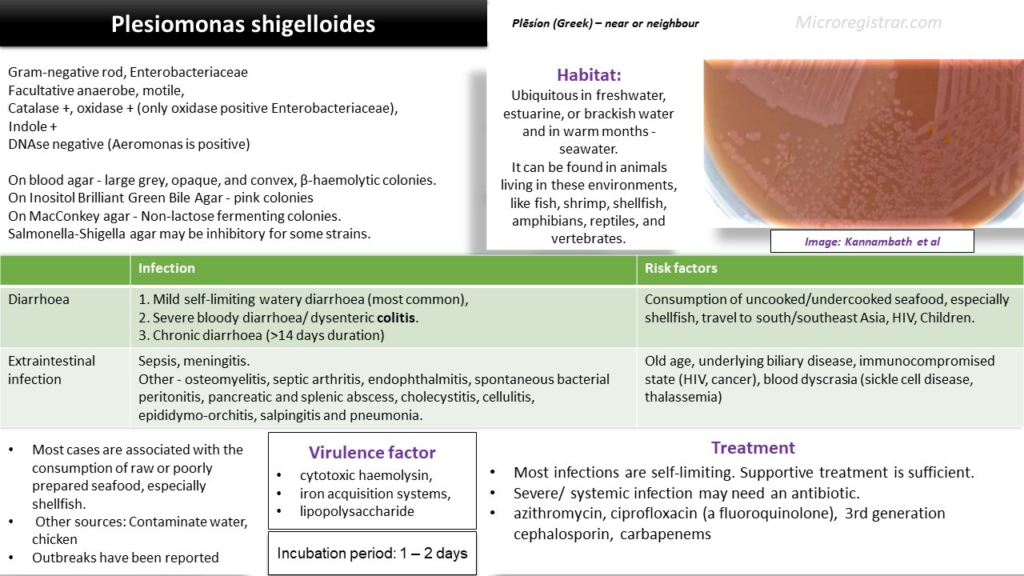
Plesiomonas shigelloides is a gram-negative bacillus that derived its name from the ancient Greek word plēsíon, which means “near” or “neighbour”, as it was considered near or related to the bacteria Aeromonas.
It is mostly found in freshwater, estuarine, or brackish water environments. It can be found in animals living in these environments, like fish, shrimp, shellfish, amphibians, reptiles, and vertebrates. It is mostly found in tropical waters but is increasingly reported in colder countries, especially in warmer months. It could also be found in seawater (and saltwater animals) in warmer temperatures.
How do we get Plesiomonas shigelloides infection?
Most cases are associated with the consumption of raw or poorly prepared seafood, especially shellfish. Other types of contaminated foods, like chicken, could also be a source. It has also been reported to occur from the consumption of contaminated water.
Plesiomonas shigelloides symptoms
Diarrhoea: Plesiomonas has been associated with diarrhoea, which could be
1. Mild self-limiting watery diarrhoea (most common),
2. Severe bloody diarrhoea/ dysenteric colitis.
3. Chronic diarrhoea (>14 days duration)
Diarrhoea could be associated with abdominal pain, fever and vomiting. It is one of the commonest causes of travellers’ diarrhoea. Diarrhoea may last from 3 to 40 days.
A large number of Plesiomonas infections ( ~30%) are co-infection with other pathogens like rotavirus, Salmonella, Aeromonas, Vibrio parahaemolyticus.
Extraintestinal infection: Infections like sepsis and meningitis are usually seen in children or in immunocompromised people. Other infections rarely associated with this bacteria are –
- osteomyelitis, septic arthritis,
- endophthalmitis,
- spontaneous bacterial peritonitis, pancreatic and splenic abscess, cholecystitis,
- cellulitis,
- epididymo-orchitis, salpingitis and
- pneumonia.
Association or risk factors
- Diarrhoea – Consumption of uncooked/undercooked seafood, especially shellfish, travel to south/southeast Asia, HIV, Children.
- Extraintestinal disease – Old age, underlying biliary disease, immunocompromised state (HIV, cancer), blood dyscrasia (sickle cell disease, thalassemia)
Virulence factors
- cytotoxic hemolysin,
- iron acquisition systems, and
- lipopolysaccharide
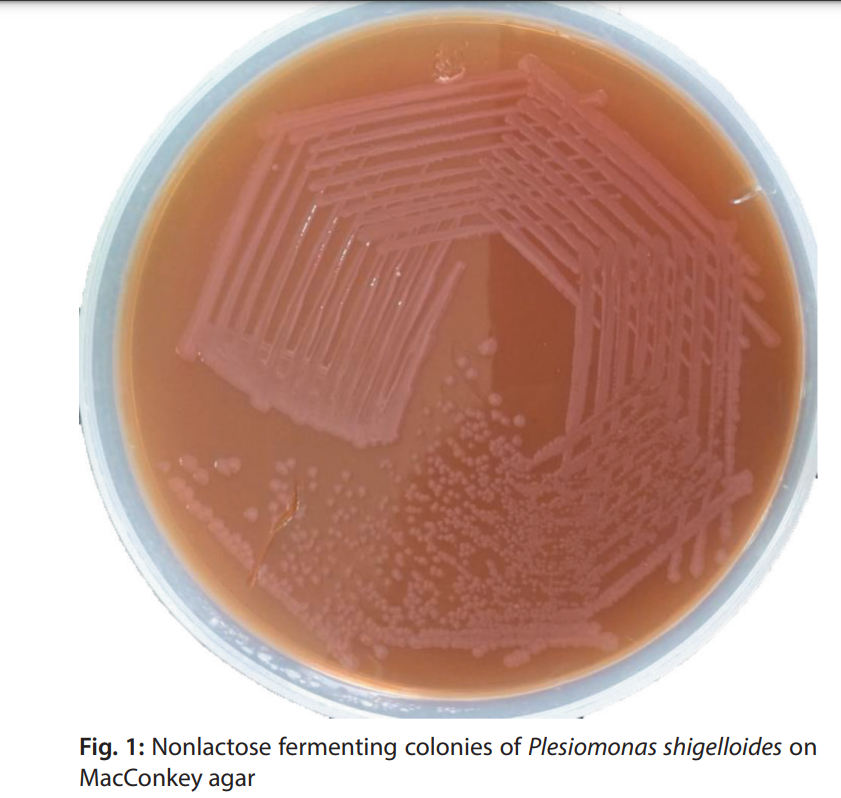
Plesimonas shigelloides laboratory identification
Gram stain: short Gram-negative rod.
It is facultatively anaerobic, non–spore-forming, motile (polar flagella) bacilli.
On blood agar, it produces large grey, opaque, and convex, β-haemolytic colonies.
On Inositol Brilliant Green Bile Agar – pink colonies
MacConkey agar – Non-lactose fermenting colonies.
Salmonella-Shigella agar may be inhibitory for some strains.
Plesiomonas shigelloides biochemical tests & other tests
It is catalase-positive, oxidase-positive, and indole-positive. It does not ferment lactose but could be variable. An oxidase test should not be performed from an enteric medium as acid production from sugars in these media can give a false negative reaction.
It is the ONLY oxidase-positive Enterobacteriaceae.
Plesiomonas is DNAse negative, while Aeromonas is positive (distinguishing feature).
Plesiomonas share antigens with Shigella sonnei and can cross-react with Shigella antisera.
Plesiomonas shigelloides Treatment
- Usually, diarrhoea is self-limiting; hence antibiotics may not be necessary. Supportive therapy with rehydration and nutrition should be sufficient.
- Chronic diarrhoea, severe disease and extraintestinal disease may benefit from antibiotic therapy.
- P shigelloides infection can be treated with azithromycin, ciprofloxacin (a fluoroquinolone), 3rd generation cephalosporin, carbapenems etc.
- This organism is often resistant to amoxicillin and tetracycline.
Reference
- Janda JM, Abbott SL, McIver CJ. 2016. Plesiomonas shigelloides revisited. Clin Microbiol Rev 29:349–374. doi:10.1128/CMR.00103-15.
- Robert M. Kliegman, Aeromonas and Plesiomonas, Nelson Textbook of Pediatrics, 2020
- Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases, 2020