Cronobacter sakazakii: pathogen from infant formula feed
What is Cronobacter sakazakii?
Cronobacter sakazakii is a gram-negative bacteria that can cause necrotising enterocolitis, septicaemia, and meningitis in infants, particularly low-birth-weight neonates. It has repeatedly been associated with reconstituted powdered infant formula. It can also cause infection in adults, especially in vulnerable groups like older people.
Infection in infants is associated with a high mortality rate (40-80 per cent). Adult infections are less severe.
What is Cronobacter sakazakii?
Cronobacter sakazakii is a gram-negative bacteria that can cause necrotising enterocolitis, septicaemia, and meningitis in infants, particularly low-birth-weight neonates. It has repeatedly been associated with reconstituted powdered infant formula. It can also cause infection in adults, especially in vulnerable groups like older people.
Infection in infants is associated with a high mortality rate (40-80 per cent). Adult infections are less severe.
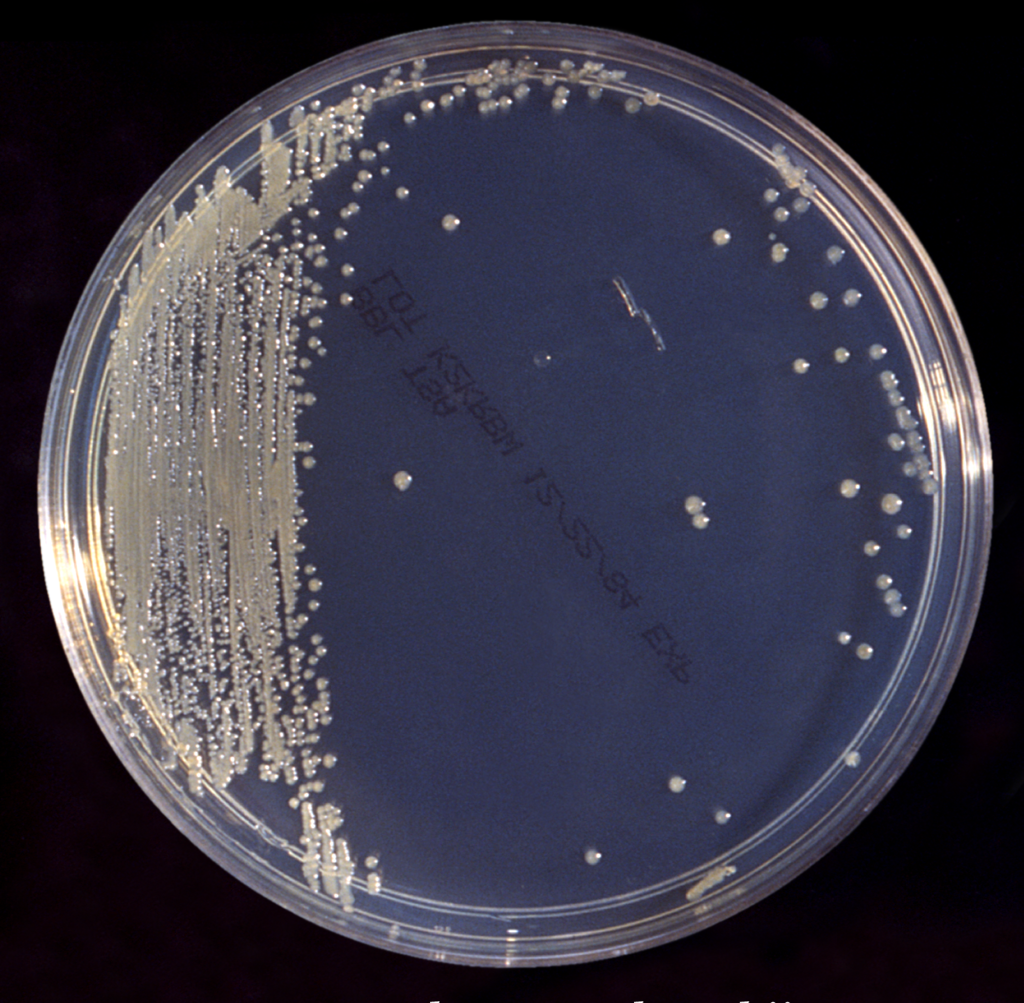
C sakazakii colonies on trypticase soy broth (TSB) agar (http://phil.cdc.gov/ ID# 6553)
It is widely distributed in the environment.
Chronobacter can withstand temperatures ranging from -5 to 47 degrees Celsius. It’s also resistant to drying, which helps it survive the formula feed’s desiccation process. Some strains of these bacteria form biofilms, which help them survive in harsh environments, such as during decontamination. According to Csorba et al., five strains were recovered from the milk powder facility, with ST4 (Sequence type 4) being the most common and prolific biofilm producer. [Csorba 2021].
These characteristics let the bacteria thrive in various habitats. It has been isolated from dry herbs, sausages, minced beef, chocolate, pasta, poultry farms, abattoirs, soil, and water. [Mahindroo, 2016]
How does Cronobacter cause infection? Virulence factors
Cronobacter is considered to be an opportunistic pathogen. However, it has few virulence factors in its arsenal, which shows the adaptation of this bacteria to its environment. It can survive in a wide range of environments due to its durability and biofilm formation.
It has beta-fimbriae that allow it to attach to inanimate objects. Apart from fimbriae, it uses a type 6 secretory system to adhere, invade, and cause disease. It can evade the immune system by multiplying inside the macrophages.
It produces various toxins like endotoxin (lipopolysaccharide), enterotoxin and cytotoxin. The outer membrane proteins ompA and ompX help it penetrate the blood-brain barrier.
Cronobacter is able to utilise sialic acid, which is an important component of the formula feed.
What disease does Cronobacter sakazakii cause?
In infants, it is known to cause meningitis, septicaemia, and necrotising enterocolitis. Cronobacter meningitis tends to be severe, associated with infarcts, necrosis, abscess, and hydrocephalus. Mortality associated with meningitis is high, up to 80%. Patients who recover are often left with neurological sequela, ventriculitis, and cerebral abscesses.
Clonal complex sequence type 4 (ST4) is strongly associated with CNS infection.
In adults, the disease tests to be milder. It can cause bacteremia, UTI, pneumonia, conjunctivitis, intraabdominal infection, wound infection, etcetera.
Laboratory identification of Cronobacter sakazakii
Cronobacter sakazakii can easily grow on non-selective media (blood agar) and selective media (VRBA)
MALDI ToF can be used to identify C sakazakii, but molecular methods are considered more reliable. Chromogenic agar [Brilliance™ Enterobacter sakazakii Agar, Chromogenic Cronobacter Isolation (CCI) Agar] and biochemical tests (API20E) have been used as well.
As this bacteria is widely available in the environment, typing methods are necessary during outbreaks. PFGE and MLST are common typing methods.


mostly*harmless, Flickr, (https://www.flickr.com/photos/21997898@N04/8508036699)
What antibiotic is Cronobacter sakazakii susceptible to?
This bacteria is resistant to macrolides, lincosamide, and fosfomycin.
In the 1980s, most of these bacteria were susceptible to ampicillin. However, resistance is increased due to the various types of beta-lactamase C sakazakii can produce, including ESBL. Resistance to amoxicillin and 1st and 2nd generation cephalosporins is common.
It has been reported to be susceptible to coamoxiclav, piperacillin-tazobactam, meropenem, cefotaxime, ciprofloxacin, and gentamicin. Some recent papers reported approx 10% of isolates resistant to cefotaxime, a 3rd generation cephalosporin (Pan, 2014).

Precaution and other points
The WHO expert committee recommends reconstituting the feed with water not cooler than 70 degrees C and consumed within 3 hours.
Powdered infant formulas should conform to international microbiological specification guidelines and be tested for Salmonella, Cronobacter etc.
In cases of an outbreak, non-food sources must also be considered potential sources, such as feeding tubes.
Reference
- O. Holý and S. Forsythe, Cronobacter spp. as emerging causes of healthcare-associated infection, Journal of Hospital Infection, 2014-03-01, Volume 86, Issue 3, Pages 169-177
- http://www.oxoid.com/culture/Culture-31-1.pdf
- Csorba et al, Prevalence, characterization, and antibiotic susceptibility of Cronobacter spp. in a milk powder processing environment: The first reported case in Serbia, Food Sci Nutr, 2021 Dec 20;10(2):554-563.
- Mahinrdroo et al, Cronobacter sakazakii – An unrecognised food borne pathogen, India, IJID, POSTER PRESENTATION| VOLUME 45, SUPPLEMENT 1, 182, APRIL 01, 2016

