Cefalexin
Nature of the antibiotic
- Semisynthetic first-generation cephalosporin.
- Oral preparation only (first oral cephalosporin introduced).
- Introduced in 1969.
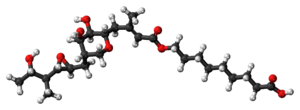
- Molecular weight – 365.41
- Cefalexin molecule is a zwitterion.
Mechanism of action
Cefalexin, like other beta-lactams, binds to the penicillin-binding protein (PBP) and prevents peptidoglycan synthesis. It prevents the formation of new cell walls and maintenance of the cell wall leading to autolysis of the bacteria due to osmotic pressure.
Mechanism of resistance
- Beta-lactamase: Secreted beta-lactamase of the gram-positive bacteria or the beta-lactamase in the periplasmic place of the gram-negative bacteria can hydrolyse cefalexin.
- Altered PBP: alteration of PBP may lead to cefalexin resistance, e.g. MRSA.
PK/PD and other properties
- Bioavailability: High. 82% at the fasting stage and 73% with food.
- Cefalexin absorption is not impaired by heart failure, achlorhydria, or partial gastrectomy.
- Protein binding: 15%
- Distribution: High in the kidney, Good concentration is inflamed lung, also found in the pancreas, liver and adrenals.
- Important parameter: Time over MIC.
- Metabolism: Not metabolised in the body.
- Excretion: Mostly kidney, <1% in bile.
- Dose adjustment: Necessary in renal impairment
- Pregnancy: Category B
Indication (cefalexin is used to treat)
- Urinary tract infections,
– including acute pyelonephritis (not as initial therapy but as oral stepdown)
– catheter-associated UTI
– uncomplicated prostatitis - Prophylaxis of recurrent urinary tract infection (unlicensed use)
– (not preferred for VUR prophylaxis, Ref – Kucer) - Diverticular disease (with metronidazole)
- Respiratory tract infections (directed therapy)
- Skin and soft tissue infections (not animal bites)
- Otitis media (directed therapy)
- OM and septic arthritis (sequential therapy)
Spectrum
Gram-positive bacteria:
| Susceptible | MSSA, Group A Streptococcus, Group B Streptococcus, Viridans Streptococcus. Corynebacterium diphtheriae and some other Corynebacterium |
| Mostly resistant | Streptococcus pneumoniae |
| Resistant | MRSA, Enterococcus |
Gram-negative bacteria:
| Susceptible | E coli, Klebsiella, Proteus mirabilis |
| Mostly resistant/resistant | Enterobacter, Serratia, Citrobacter Proteus vulgaris, Providentia, Morganella, Campylobacter Haemophilus, Moraxella Pasteurella Pseudomonas aeruginosa |
Anaerobes:
| Susceptible | Peptococcus, Peptostreptococcus |
| Maybe susceptible | Prevotella, Porphyromonas Fusobacterium |
| Resistant/mostly resistant | Clostridium Bacteroides |
Adverse effects
- Gastrointestinal adverse effects
- Eosinophilia, neutrophilia, leucopenia, thrombocytopenia
- Skin reaction (rash, erythema multiforme, SJS), vulvovaginal candidiasis
- Headache
- Rare/less common: Anaphylaxis, C difficile diarrhoea, tubointerstitial nephritis