Rothia mucilaginosa
The Bacteria
Rothia belongs to the family Micrococcaceae – the same family as Micrococcus spp., Stomatococcus spp. and Kocuria spp.
There are 8 species of Rothia – but only Rothia dentocariosa and Rothia mucilaginosa has been associated with human disease.
It is a member of the mouth and upper respiratory tract flora.
Laboratory
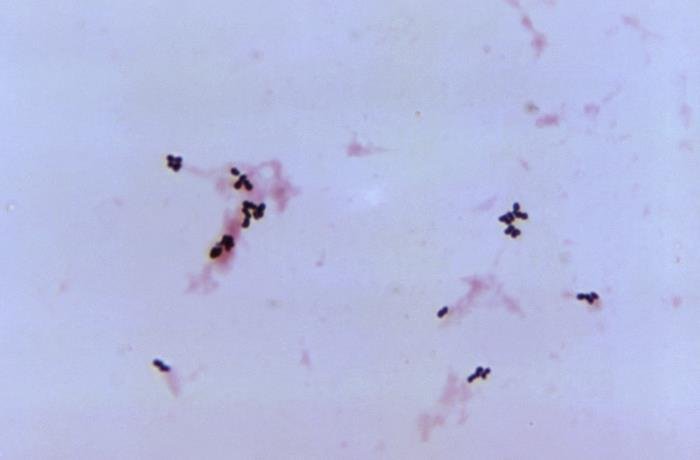
- Gram-positive cocci may appear singly, in pairs, clusters, or chains – mostly pairs/clusters. However, Microcolonies on agar surfaces are composed of filamentous branched elements which rapidly fragment into bacillary or coccoid forms, resembling Actinomyces or Nocardia species [PHE SMI].

- Grow in aerobic or microaerophilic conditions but not anaerobically
- Weakly catalase-positive or catalase variable
- Oxidase-negative
- Colony – on blood agar clear/white, nonhemolytic, mucoid/sticky colonies – adherent to the agar surface
- It is susceptible to bacitracin and hydrolyses aesculin
- Unable to grow in the presence of 5% sodium chloride.
Infection
Rothia is an opportunistic pathogen and has been reported to cause –
- Bloodstream infection
- Skin and soft-tissue infections in children
- CNS infection – meningitis
- Pneumonia
- Necrotizing fasciitis
- Prosthetic joint infection
- Endocarditis and
- Peritonitis
Risk factors for Rothia infection – Immunocompromised state or some form of breach in host defence is associated with Rothia infection. A case series suggested a significant association was seen with steroid use (81% versus 13%; P= 0.0014) and fluoroquinolone use (86% versus 13%; P≤ 0.0001) preceding bacteremia in neutropenic patients. [Abidi, 2016]
Other risk-factors
- leukaemia
- solid tumour
- neutropenia
- Central venous access
- valvular heart disease
- continuous ambulatory peritoneal dialysis and
- intravenous drug abuse (IVDU)
- dental and head-neck surgery
Treatment
Rothia is uniformly susceptible to vancomycin (glycopeptides).
It is also sensitive to penicillin, amoxicillin, tetracyclines, rifampicin, 2nd/3rd generation cephalosporins, and carbapenems.
Following drugs tend to have higher MIC – fluoroquinolones, aminoglycosides, co-trimoxazole, erythromycin, clindamycin and fosfomycin.
There is no specific EUCAST/CLSI standard, but EUCAST non-species specific breakpoints can be used (Ekkelenkamp, Staphylococci and micrococci, Infectious Diseases 3e).
Glycopeptides are usually used in treatment, but combination therapy (beta-lactam with rifampicin/aminoglycosides) has also been reported.


