Corynebacterium macginleyi – an under-reported cause of conjunctivitis
Corynebacterium macginleyi (CM) is lipophilic, slow-growing, gram-positive bacteria first described in 1995 and was named after Kenneth McGinley, who made an essential contribution to the field of lipophilic coryneform bacteria.
CM has been associated with conjunctivitis and other eye-related infections. It has also been implicated in various non-ophthalmic infections as an opportunistic pathogen.
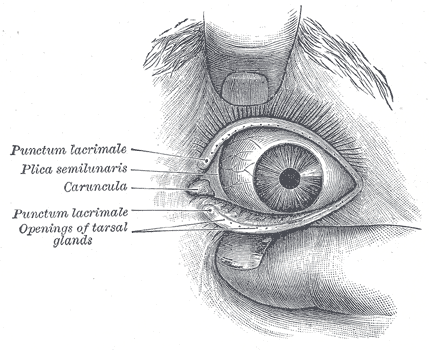
It has been proposed that CM is a conjunctiva-specific pathogen that colonises the lipid-rich environment of the meibomian glands/tarsal glands.
Corynebactrium spp.
Corynebacterium is an aerobic gram-positive, non-motile rod, often with clubbed ends but could be pleomorphic. In gram stain, it may stain unevenly and appear beaded. They group in a characteristic way, which has been described as the form of a “V”, “palisades”, or “Chinese letters”. Metachromatic granules are usually present representing stored phosphate regions.
Corynebacterium are facultative anaerobe or aerobe and may grow slowly. On blood agar, they produce small greyish colonies.
Selective and differential media for Corynebacterium is Hoyle’s tellurite medium.
Three species of Corynebacterium, C. diphtheriae, C. ulcerans, and C. pseudotuberculosis, carry the phage borne diphtheria tox gene, which is required to produce toxin. These three species are capable of causing diphtheria or diphtheria like illness.
Other diphtheria species are usually the commensals of the skin and mucous membrane but can be opportunistic pathogens.
Diseases associated with C macginleyi
Most cases of CM have been associated with eye infections –
conjunctivitis,
keratitis,
corneal ulcer,
preorbital cellulitis,
blebitis and
endophthalmitis
[Sagerfors, Nature 2021][Fong, Pathology 2021].
CM has also been reported from various non-ocular infections. For example –
catheter-related urinary tract infection,
catheter-related blood-stream infection,
endocarditis,
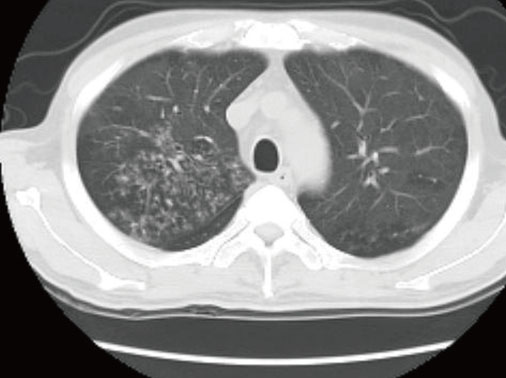
pneumonia in an HIV-infected individual or ventilated patient,
tracheostomy site infection in a patient with laryngeal carcinoma and
post orthopaedics surgery surgical site infection.
Co-infection-
In many ophthalmic cases (approx 50%), other pathogenic bacteria and viruses have also been isolated from the clinical specimens. The most common associated bacteria was Staph aureus.
Risk factors –
Eye – Contact lens, a breach in epithelial surface,
Extraocular – prosthetic material, immunocompromised state (HIV, malignancy)
Laboratory identification
Gram stain – typical of Corynebacterium spp. (see above)
Colonies – On blood agar, CM produces very small (<1mm diameter) nonhaemolytic colonies after 48 hrs (large reddish-beige colonies can be seen when blood agar is supplemented with Tween-80).
Tests – catalase positive, oxidase negative, nitrate is reduced to nitrite, urease negative. [Riegel 1995]
Final identification can be made using – MALDI-ToF (reliable identification), API coryne, 16S rRNA sequencing supplemented with rpo B gene sequencing.
Many isolates are likely classed as contaminants and not followed up/reported.

Treatment
The reported susceptibility varies –
Sagerfors et al. reported CM susceptible to benzylpenicillin, vancomycin, gentamicin, ciprofloxacin and moxifloxacin. Chloramphenicol susceptibility was variable based on MIC.
Fong et al. reported all the isolates were susceptible to vancomycin, ciprofloxacin and linezolid. Susceptibility to clindamycin, penicillin and tetracycline was variable.
Eguchi et al. reported high-level fluoroquinolone resistance from Japan, which could be specific to the country or population group.
Funke et al. reported that C. macginleyi is uniformly susceptible to penicillins, quinolones, and aminoglycosides.
Reference
Fong et al, Corynebacterium macginleyi in the era of MALDI-TOF MS: epidemiology, susceptibility patterns and prevalence of co-infection, Pathology (article in press)